A ocitocina, hormônio produzido no cérebro e ligado a funções corporais, como o parto e a produção de leite em mulheres, e a relações sociais, como a ligação entre pais e filhos, pode virar tratamento contra autismo. Pessoas com o transtorno têm dificuldade de reconhecer expressões faciais e de criar laços sociais.
O psiquiatra James Leckman, que veio a São Paulo no mês passado, a convite do Instituto de Psiquiatria da USP, está pesquisando o efeito da ocitocina em autistas.
O psiquiatra James Leckman, que veio a São Paulo no mês passado, a convite do Instituto de Psiquiatria da USP, está pesquisando o efeito da ocitocina em autistas.
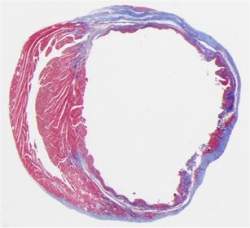
Arte/Folhapress
O médico, que é professor de psiquiatria infantil em Yale, participa de estudo em que voluntários recebem doses de ocitocina e terão seus cérebros examinados em testes de imagem. A pesquisa ainda está em andamento.
Mas trabalhos anteriores com o hormônio mostram que doses intranasais de ocitocina podem melhorar as habilidades sociais do autista.
Um estudo publicado no ano passado na revista "PNAS" descreve os efeitos da ocitocina em um grupo de pessoas com autismo.
O hormônio melhorou o reconhecimento de expressões faciais e a habilidade de interação dos voluntários com autismo em jogo virtual.
Outro exercício exigia que os participantes olhassem para expressões faciais em um computador e identificassem se o rosto era de homem ou mulher e a direção que os olhos apontavam.
Autistas, antes do tratamento com ocitocina, olhavam pouco para o rosto representado na imagem. Após as doses de ocitocina, conseguiram fixar mais seu olhar.
O resultado sugere que a ocitocina reduza a ansiedade dos autistas na hora de fazer contato visual.
Segundo Leckman, ainda é necessário fazer mais testes para determinar se o tratamento é seguro e eficaz. "É diferente ler expressões faciais em um teste e na vida real. Também não se sabe se o hormônio vai fazer diferença a longo prazo."