|
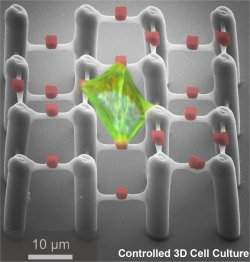
Ciona allows scientists to study in detail how cells interact to build complex organs. In this microscopic image, two of the cells that will form the heart were stained with a green fluorescent marker and can be seen in the lower portion of the tadpole-like Ciona embryo. |
"We still don't know much about the causes of many of these defects. Some have been linked to certain genes but the picture is still sketchy," he says. "At this point, we can't predict how children will respond to current methods, but if we had genetic indicators we could use them to personalize treatments."
Dr. Ricardo Samson, who heads the pediatric cardiology section at the College of Medicine, adds that "some heart defects can be difficult to diagnose because they don't present the typical signs such as a heart murmur or blueness of the skin."
"Fortunately, prenatal ultrasound allows obstetricians to identify many babies with specific forms of severe heart defects before they are born," he says. "But because of the way the heart develops in a fetus, some severe defects go undetected and don't cause problems until the baby has gone home from the nursery."
Samson and Klewer both are members of the UA's Steele Children's Research Center and the UA's Sarver Heart Center's heart development research group, which is internationally recognized for its discoveries expanding the understanding of molecular elements that cause congenital heart defects.
In studying heart-specifying genes, less is more
Studying the genetic underpinnings of heart defects is complicated by the fact that humans, like all other vertebrates, have multiple and slightly different copies of each gene. This redundancy makes it difficult if not impossible to tease apart the functions associated with a particular gene, because disrupting its function in model organisms such as mice to figure out its role does not always result in an obvious effect.
In their quest to better understand and help clinicians develop better diagnostics and treatments for congenital heart defects, scientists at the UA's department of molecular and cell biology have turned to a creature most people -- with the possible exception of scuba divers -- would not consider a familiar sight: a sea squirt in the genus Ciona.
Lacking a head, appendages and eyes, sea squirts resemble strange-looking, leathery sacks more than animals. Up to 6 inches long, with two conspicuous openings, Ciona spends its life attached to submerged rocks or piers, pumping sea water through its body and straining out food particles, much like clams do. Its simple body structure, however, belies the sea squirts' biological kinship, which places them closer to the vertebrate lineage than any other invertebrate. Most importantly, Ciona's genetic blueprint is almost the same as that of vertebrates.
"We want to understand the basic processes by which embryonic cells make the decision to become heart cells," says Brad Davidson, an assistant professor in the UA's department of molecular and cellular biology and a member of the Sarver Heart Center. "Early steps of heart formation are very similar in Ciona, mice and humans."
Except -- and for a scientist studying heart development, this is huge -- each of Ciona's genes is represented only once because the genome has not been duplicated as in vertebrates. Therefore, Ciona has only one copy of the major genes involved in heart development.
One of the genes vital for heart development is GATA, a so-called transcription factor or master gene that controls other heart-specific genes and plays a key role in heart development. Human babies with GATA mutations have congenital heart defects. If the gene's function is disrupted, both the heart and the gut are deformed.
"But it's not clear where the problem is," Davidson says. "Is it because the heart doesn't form properly or because the gut doesn't form properly? Ciona allows us to break it apart."
IMAGE: This is Katerina Ragkousi, the first author of the research report, with principal investigator Brad Davidson.
Click here for more information.
A heart needs a gut
"We tend to think of cells building an organ as an isolated process but that is never true in an embryo," he says. "Anything that is being built has to be made alongside all the other organs, and there are a lot of complications in terms of the instructions."
Katerina Ragkousi, a postdoctoral fellow in Davidson's lab, just published the results of a study shedding light on this process in the journal Developmental Biology. The editors deemed her work important enough to feature it on the cover of the magazine.
"We know that in vertebrates, GATA has to be activated not only in the future heart cells, but in the neighboring gut cells, too," Ragkousi says. "In this study, we show that this is the same in Ciona, justifying even more the value of this model organism in studying heart development."
"Vertebrates have three GATA factors that are both in the developing gut and in the heart, so it has been really difficult to tease apart what's going on with these factors in each tissue."
When Ragkousi and her team experimentally disrupted GATA in heart precursor cells, the cells lost their identity.
"They don't express the right genes and stay in a state of limbo instead of moving on with their development," Davidson said.
"When we disturb GATA function independently in the developing gut, we see that heart cell identity is not perturbed, at least not at this stage," Ragkousi says. "However, we find that GATA in the gut plays an indirect role in heart formation in that it is necessary for heart precursors to be properly positioned in the developing embryo."
In addition to its genetic similarity to vertebrates, Ciona comes with several other benefits. It is easy to keep in the lab, and, unlike vertebrate embryos, a Ciona embryo consists of a mere few hundred cells. The embryos develop in only 24 hours and are translucent, allowing scientists to literally watch as the heart forms from only four cells.
"It is this simplicity that we are hoping to be able to exploit," Davidson says. "That we can not only see vaguely and in general how the cells build a heart, but very specifically how each cell is acting as they come together to make the heart."
In their natural habitat, Ciona embryos drift along with the ocean currents until they hatch as tiny, tadpole-like larvae.
"They need to develop rapidly because until they hatch, they're floating around as food," Davidson says. "Sometimes it can take days for them to settle. They can stay alive for five or six days. In the right kind of current, they can go pretty far."
Once the larvae come to rest on the seafloor, a rock or a pier, they undergo one of the most dramatic metamorphoses found in the natural world. Giving their body a total makeover, they morph from a free-swimming larva with a brain, primitive eyes and a tail into the sponge-like sack that spends remainder of its life attached to the very place it settled down.
"With Ciona, we can introduce genes into the early embryo and as it develops, we can study where the genes are expressed," Ragkousi says. "We also can locate the cells relative to each other. We are looking at the cellular interactions that happen during the early stages heart formation. It has been almost impossible to address this at such a high resolution and study the behavior of individual cells in more complex organisms."
Bench-to-bedside medicine, or from the water tank to the hospital
"Basic research with model organisms like Ciona allows us to identify the genes involved in heart development and recognize who the players are," says Klewer. "We can then look at these factors in patients to determine the best approach for treatment that would benefit that particular patient. It also gives us an opportunity to refine our approaches based on the genetic background. I am hopeful that we can soon integrate that knowledge in our clinical practice."
Researchers studying heart development put high hopes in Ciona not only to improve diagnostic tests through a better understanding of the genetic mechanisms underlying heart development, but also to develop better therapeutics for failing hearts.
"Many people are going to have a heart attack at some point in their lives," says Davidson. "And since the heart can't regenerate damaged tissue, what do you do to manage that? There is a big push to see if we can reprogram cells to build heart tissue. Progress is being made, but there are a lot of stumbling blocks to figuring out how to do that right. One of the keys is to make sure the cells that doctors put into a damaged heart behave like heart cells and not like cancer cells and don't do the wrong things."
Klewer adds: "In the future, clinicians will have more options for successfully performing surgery on a fetus. But they can't do that unless they know there is a problem. This approach holds the promise of correcting a heart problem early, and allow for more normal heart growth and function during development, which might save an affected child from a lot of complicated procedures that otherwise would be needed after birth."