Desativação de hormônio dispensaria injeções de insulina, dizem cientistas. Testes pré-clínicos foram feitos em camundongos.
Uma equipe do Centro Médico da Universidade do Sudoeste do Texas, nos Estados Unidos, sugere que a desativação de um hormônio pode ser suficiente para tratar diabetes tipo 1, uma doença autoimune - na qual o sistema de defesa ataca as células e tecidos do próprio corpo -, que faz as concentrações de açúcar no organismo ficarem muito altas. A descoberta será tema de edição de fevereiro da revista especializada "Diabetes".
Liderados por Roger Unger, professor da instituição e principal autor do artigo científico, os pesquisadores testaram a capacidade de camundongos, cobaias comuns em testes pré-clínicos, aproveitarem o açúcar presente no sangue, fruto da alimentação dos animais.
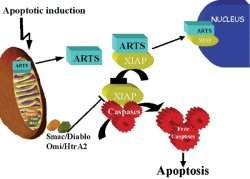
No caso dos diabéticos, essa ação do glucagon faz os níveis de glicemia aumentarem muito. Esse efeito seria compensado em pessoas saudáveis pela ação da insulina, responsável por permitir que o açúcar penetre nas células do corpo. Dentro delas, a glicose poderia ser imediatamente aproveitada para gerar energia ou armazenada. Mas para os pacientes com diabetes tipo 1, a produção de insulina não existe ou é seriamente comprometida.O truque foi alterar geneticamente os roedores para que produzissem quantidades menores de uma substância conhecida como glucagon, responsável por impedir que os níveis de glicose (açúcar) fiquem muito baixos.
Mas os pesquisadores norte-americanos acreditam que os resultados obtidos com os camundongos apontem que, caso os níveis de glucagon consigam ser controlados, a insulina se torna supérflua, já que os níveis de glicemia estariam normais, dispensando as injeções da substância para equilibrar a "balança" do açúcar no sangue.
Batalha de hormônios
A insulina deixa de existir em pacientes com diabetes tipo 1 pois o sistema de defesa do corpo ataca 90% ou mais das células beta, estruturas localizadas em uma região do pâncreas conhecida como Ilhotas de Langerhans. Com a ausência da insulina, os níveis de glicemia no sangue não abaixam e não há ação para impedir a influência do glucagon.
O "padrão ouro" de tratamento da doença é por meio de injeções de insulina, desde a descoberta da doença, em 1922. Os pacientes precisam receber as doses da substância durante boa parte da vida. No universo de todas as formas de diabetes, o tipo 1 responde por 10% dos casos e a maior parte das pessoas com o desenvolve antes dos 30 anos.